#WorldLiverDay #FoodIsMedicine
Food is medicine - World Liver Day 2025
“In adults with Metabolic Dysfunction-associated Steatotic Liver Disease (MASLD), dietary and behavioural therapy are essential for improving liver injury and preventing advanced liver disease and hepatocellular carcinoma (HCC). Sustainable lifestyle interventions, accessible and affordable to patients, should be emphasised by healthcare professionals while being sensitive to stigma, socioeconomic factors, and cultural differences. Effective weight loss strategies, including caloric restriction and increased physical activity, should be tailored to individuals’ needs. Adherence to the Mediterranean diet, which restricts unhealthy foods, can prevent MASLD and lower the risk of developing HCC, supported by an interdisciplinary approach to enhance treatment coordination. Overall, promoting healthy eating patterns and regular physical activity is crucial for reducing the risk of liver-related diseases.”
Prof. Shira Zelber-Sagi, EASL Public Health Councillor
Every year on 19 April, World Liver Day aims to raise awareness about liver health, prevention strategies, and the growing burden of liver diseases worldwide. It serves as a global call to action, emphasising the importance of prevention, early detection, and lifestyle changes to fight conditions like metabolic dysfunction-associated steatotic liver disease (MASLD), liver fibrosis, and liver cancer.
This year’s theme, “Food is medicine”, highlights the powerful role of diet protecting and restoring liver health. A balanced diet rich in whole foods such as, fruits, vegetables, whole grains, and lean proteins, not only improves liver function but also helps prevent and even reverse liver disease.
However, for many, healthy eating is neither accessible nor affordable. Policies and commercial influences shape food environments, often making nutritious choices harder to reach. While these factors often lie beyond individual control; one powerful step you can take is to stay informed about how your diet impacts your liver health. Small intentional changes to your lifestyle can make a meaningful difference over time.
“Healthy foods, smarter choices. Calling for global action.”
Prof. Aleksander Krag, EASL Secretary General
Preventive hepatology: the role of nutrition in liver health
Liver disease is a global leading cause of death and illness, mainly caused by unhealthy lifestyle habits. However, most liver diseases are preventable. Research shows that approximately 90% of serious liver diseases are caused by asymptomatic viral hepatitis or exposure to unhealthy food, alcohol and lack of active lifestyle that lead to liver fat accumulation (Bhadoria et al., 2023). Maintaining a healthy diet and performing regular exercise can significantly reduce chronic liver disease and liver cancer.
The Mediterranean diet – with or without calorie restriction – has been extensively studied for its therapeutic benefits in MASLD. This diet encourages the intake of olive oil, vegetables, fruits, nuts, legumes, whole grains, and seafood while limiting portions of processed meats, added sugars, and refined carbohydrates. Due to its rich content of polyphenols and healthy fats, the Mediterranean diet enhances liver health. Studies have shown that, when combined with exercise, it can significantly reduce liver fat, improve metabolic markers, and increase compliance with other dietary therapies. The Mediterranean diet provides a strong foundation, on which dietary patterns can be adjusted to individual requirements as long as core nutritional principles are maintained (Zelber-Sagi et al., 2022). A recent study on French patients with liver cirrhosis found that 42.5% had insufficient fruit and vegetable intake (Manneville et al., 2025), which is a missed opportunity since consuming more than 240 g/day of vegetables was linked to a 65% reduction in hepatocellular carcinoma (HCC), incidence.
If you're looking for healthy recipes to nourish your liver, have a look at the recipe book below, test them and tag your photos using #WorldLiverDay!
Beyond nutrition, regular physical activity is essential for maintaining liver health. Research shows that daily physical exercise and caloric restriction significantly improve hepatic health (including reduction of liver fat and inflammation) by, most likely, redirecting excess nutrients into skeletal muscle and reducing hepatic nutrient toxicity (Mucinski et al., 2024). They also induced significant reductions in body weight, fat mass, and improved cardiorespiratory fitness (VO2 peak). Researchers suggest that clinical guidelines should prioritise aerobic exercise, as included in the 2024 EASL–EASD–EASO Clinical Practice Guidelines on MASLD, as a fundamental component of liver disease management in patients with advanced metabolic dysfunction-associated steatohepatitis (MASH), since it offers the greatest liver fat reduction as well as cardiovascular (heart disease prevention) benefits. Resistance training is also important as it can reduce liver fat and improve muscle mass.
Food inequity and liver disease
Social determinants such as income, education, and access to medical care play a crucial role in determining who is most at risk and who receives proper treatment. Individuals from lower-income or disadvantaged groups are often more at risk due to limited access to viral hepatitis testing, vaccination, treatment, and disease management. Additionally, alcohol-related liver disease and MASLD are more prevalent in economically disadvantaged communities due to poor access to medical care and unhealthy food environments. This socioeconomic disparity is also associated with increased intrahepatic lipid content (Ren et al., 2023). Low physical activity, dietary fiber intake, and high fructose consumption from sweetened drinks may partially explain this association. Broader societal interventions are needed to reduce the burden of MASLD (Zelber-Sagi et al., 2024), and future studies should investigate other contributing factors beyond traditional lifestyle components.
Studies also highlight the strong link between food insecurity and MASLD prevalence (Younossi et al., 2025; Zelber-Sagi et al., 2024). In high-income countries, food insecurity is related to high MASLD rates, probably by increased consumption of ultra-processed and low-quality foods, aggressive marketing of unhealthy foods, and limited availability of nutritious options. Addressing these challenges requires multi-level interventions, including improved food policies, healthcare access, and community-based initiatives like "Food is Medicine" to reduce the global MASLD burden.
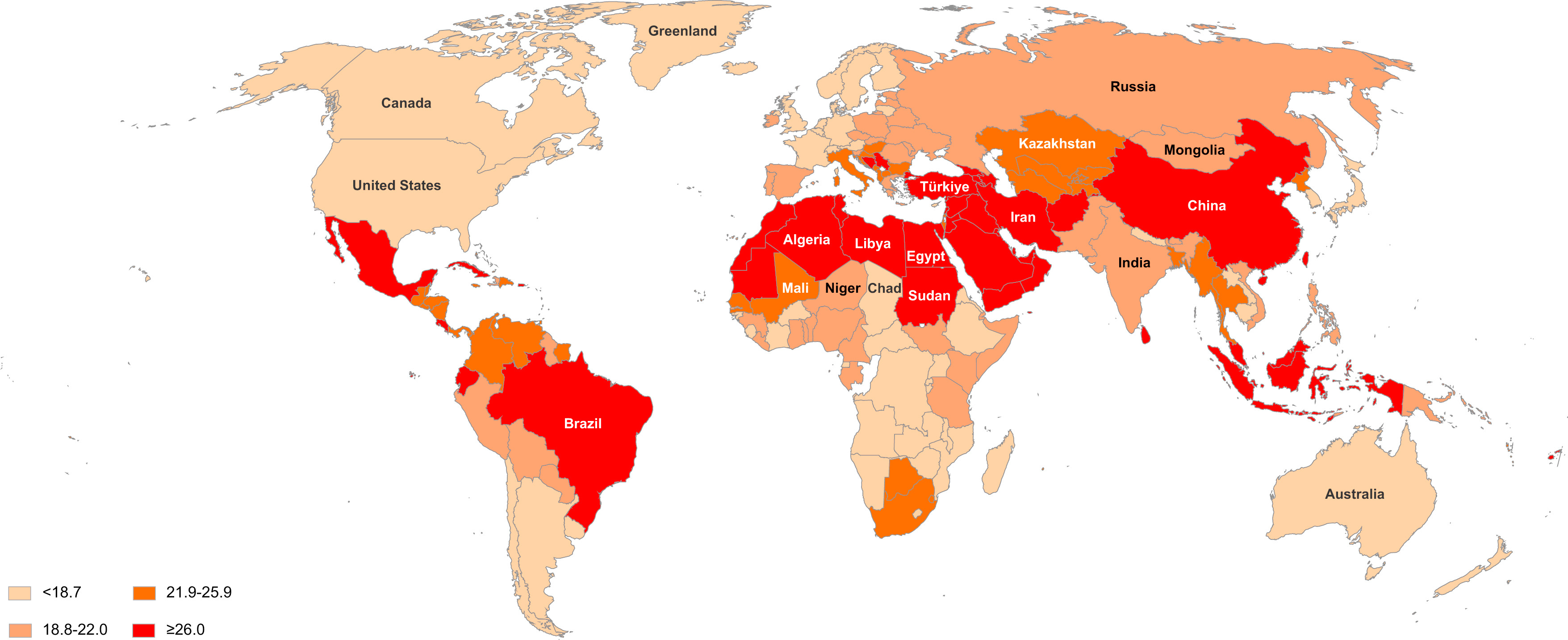
Figure 1: Global heat map of MASLD prevalence (%) in 2021 (from Younossi et al., 2025).
Obesity and liver disease: a growing public health crisis
World Obesity Day was observed on 4 March 2025, highlighting the urgent need for action against the global obesity epidemic. Obesity is a major risk factor for MASLD, and as obesity rates continue to rise, so does the prevalence of liver disease, often progressing silently until severe complications like cirrhosis or liver cancer develop. Urgent public health actions, such as improved healthcare access, policy changes, and lifestyle interventions, are needed to combat this epidemic.
The HEPAHEALTH II study used a microsimulation model to assess the impacts of alcohol and obesity policy interventions on chronic liver disease and liver cancer in Europe (Retat et al., 2024). The study suggested that a minimum unit pricing (MUP) of €1 on alcohol would reduce the incidence of liver disease significantly, and a package of an MUP of €0.70 and a sugar-sweetened beverage tax could reduce the burden as well (Figure 2). The findings highlight the importance of comprehensive policies on alcohol consumption and obesity to prevent liver disease.
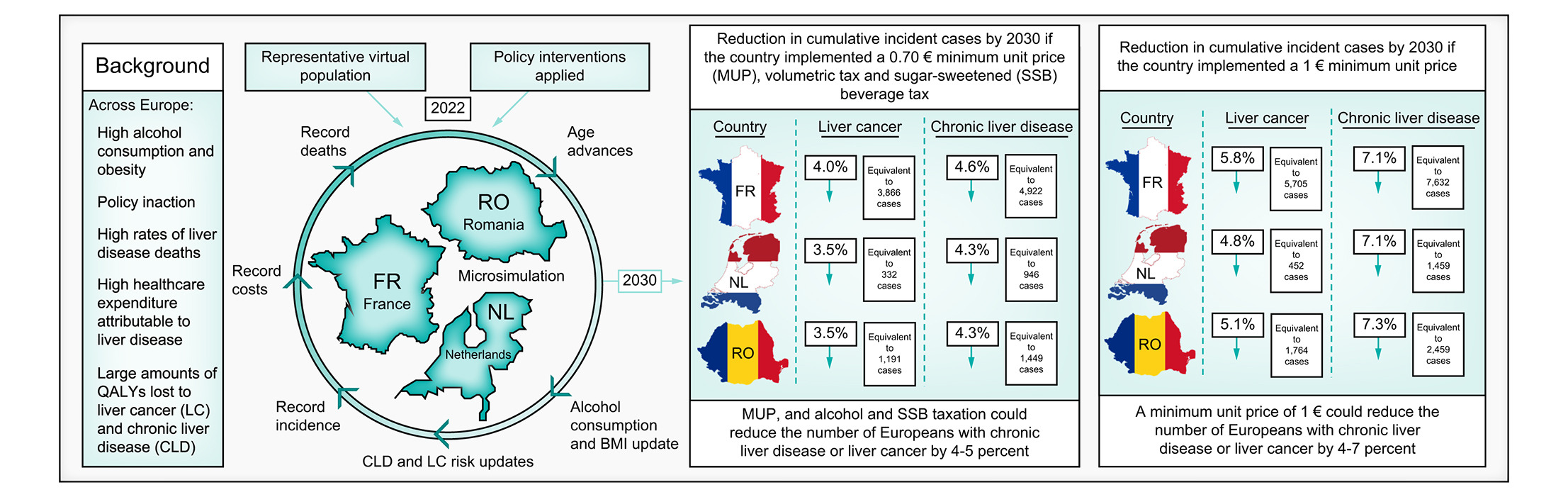
If you are eager to learn more, check out the EASL Studio "The impact of policy measure in preventing liver diseases: The Hepahealth II study", the EASL Policy Dialogue "Preventing liver disease with policy measures: The Hepahealth II study" and read the paper "Preventing liver disease with policy measures to tackle alcohol consumption and obesity: The HEPAHEALTH II study" in the Journal of Hepatology.
EASL’s commitment to liver health
EASL-Lancet Commission
Triggered by the rising burden of liver disease, the Lancet and EASL jointly arranged a Commission to explore the landscape of liver health in Europe. Published in 2021, the first report identified key challenges in tackling the increasing health burden of liver disease and provided ten evidence-based recommendations promoting a paradigm shift within liver care. This shift aims to encourage and facilitate the liver community in moving away from end-stage care and towards disease prevention and health promotion. In November 2023, a second EASL-Lancet Commission began with the goal of creating a roadmap for the operationalisation of the recommendations set forth in the first report.
Official launch of the EASL–Lancet Liver Commission report on liver disease in Europe
Healthy Livers, Healthy Lives Coalition
AASLD (American Association for the Study of Liver Diseases), ALEH (Latin American Association for the Study of the Liver), APASL (Asian Pacific Association for the Study of the Liver), and EASL are the founding members of Healthy Livers, Healthy Lives: a global coalition for action which is a catalyst to drive action across the clinical, public health and policy level.
The coalition is a platform through which the Founding Members and partners collaborate on issues of global relevance where a united voice is needed to deliver change. The coalition originates from several years of work on MASLD, the range of activities and scope of issues covered may adapt over time as decided by the Council/Steering Group.
EASL Clinical Practice Guidelines and Policy Statements
EASL plays a crucial role in shaping liver health policies and clinical guidelines to address the growing burden of liver disease. The EASL Clinical Practice Guidelines (CPGs) and policy statements provide evidence-based recommendations for the prevention, diagnosis, and management of conditions like MASLD and alcohol-related liver disease (ARLD). Key guidelines, such as the 2024 EASL–EASD–EASO CPGs on MASLD, highlight the intersection of metabolic health and liver disease, while earlier policy statements emphasize the impact of obesity and alcohol consumption on liver health across Europe. These guidelines serve as essential tools for healthcare professionals, policymakers, and researchers in promoting preventive hepatology and equitable liver care.
• Obesity is feeding the rise in Non-Alcoholic Fatty Liver Disease (NAFLD) across Europe, 2019
If you want to know more about how alcohol impacts the liver, check out the article “Dry January: an opportunity to rethink alcohol consumption”.
Make your impact
Awareness is the first step toward better liver health for all. This World Liver Day, you can make a difference by spreading the word, engaging in discussions, learning about liver disease prevention, and supporting research initiatives that improve patient outcomes.
You can find below all EASL resources and events.
Resources
EASL Quiz
• 3 questions and other EASL Quiz questions related to “Metabolism, alcohol and toxicity” to test your guidelines knowledge;
EASL DeepDive
• Glucagon in MASH: A next step in “metabolic” drugs tackling liver disease?;
EASL Studio episodes
• LITMUS: Defining the colour of NAFLD;
• Special Edition: Highlights of EASL NAFLD Summit 2022;
• Ending fatty liver disease as a public health threat;
• NAFLD and NASH – moving beyond the liver biopsy – where are we now?;
• The conundrum of NASH: The growing global disease burden with low disease awareness;
• JHEP Live: New and promising drugs for NASH on the horizon;
• Are 30% of the global population sick? A critical view on Steatotic Liver Disease and care pathways;
• JHEP Live: The new nomenclature for SLD: A multidisciplinary evaluation and approach;
• Why bother with diet and exercise when an injection will suffice?;
• Why should diabetologists care about the liver?;
• Do we solve MASLD by treating obesity?;
• The impact of policy measure in preventing liver diseases: The Hepahealth II study;
• Resmetirom: First approved drug for MASH, for whom and for how long?;
• EASL Studio Elsewhere: Spotlight on Steatotic Liver Disease at INASL 2024;
• The changing face of Steatotic Liver Disease: Navigating new opportunities and emerging challenges;
• Why does WHO engagement with Steatotic Liver Disease matter?;
• 2025 Update on Steatotic Liver Disease: Rethinking standard of care;
• Fats or carbs, who is the real villain?;
• Bugs and the liver - The role of the gut microbiome in liver diseases;
• Promoting Liver Health: An urgent call for action at WHO;
• Why bother with diet and exercise when an injection will suffice?;
• Why should diabetologists care about the liver?;
• Do we care enough about the importance of DILI/DHILI?;
• The liver as a master regulator of ageing, health, and longevity.
EASL Studio Live at EASL Congress
• SLD nomenclature: Need for refinement? (2024);
• MASLD anno 2024: A rapidly changing landscape (2024).
EASL Policy Dialogues
• Fatty liver disease: The approaching tsunami in NCDs;
• Diagnosing Steatotic Liver Disease – Challenges and opportunities;
• Preventing liver disease with policy measures: The Hepahealth II study;
• Protecting our children: Junk food & liver disease;
• World Liver Day (2023);
• World Liver Day – Join us in celebrating liver health on a global scale (2024).
Policy webinar
• Steatotic liver disease – the missing piece in the NCD puzzle.
EASL Journal Club
Online courses
• EASL-ESPEN nutrition in liver diseases;
• EASL Postgraduate Course 2021: Lifestyle and the liver.
Webcasts
• Nutrition in advanced liver diseases (EASL Congress 2023);
• Nurses & AHPs Forum: The burden of liver disease: prioritising symptom management to optimise nutritional intake (EASL Congress 2023);
• Epidemiology, disease modifiers and models of care (NAFLD Summit 2022).
Upcoming events
May 2025
EASL Congress 2025, 7-10 May in Amsterdam
Thursday, 8 May
• MASH therapy present and future: Should we target metabolic dysfunction or fibrogenesis?
• EASL/EASD Do's and don'ts in the management of MASH
• Meet-the-Experts - Management of MetALD patients in 2025
Friday, 9 May
• Future of Hepatology: Novel therapeutics and evolving challenges in managing MASLD
• EASL/EASO Meet-the-Experts: Anti-Obesity treatment: what effect can we expect on MASLD?
• Meet-the-Experts: GLP1-RA versus bariatric surgery in compensated MASH cirrhosis
• EASL Studio Season 8, Episode 11 “Interprofessional Session: Implementing the New EASL MASLD Guidelines into Clinical Practice” 21 May 2025, 18:00 CEST.
June 2025
• EASL Studio Season 8, Episode 14 “EASL Studio episode on SLD”, 11 June 2025, 18:00 CEST.
• EASL DeepDive session "MASLD Guidelines implementation" on Wednesday 25 June 2025 at 18:00 CEST.
Articles and references
Bhadoria AS et al. Preventive hepatology: An ounce of prevention or pounds of cure to curb liver diseases. J Family Med Prim Care. 2023 Mar;12(3):419-421. doi: 10.4103/jfmpc.jfmpc_2225_22.
Zelber-Sagi S et al. Food inequity and insecurity and MASLD: burden, challenges, and interventions. Nat Rev Gastroenterol Hepatol. 2024 Oct;21(10):668-686. doi: 10.1038/s41575-024-00959-4.
van Amsterdam J and van den Brink W. Sweet-liking and sugar supplementation as innovative components in substance use disorder treatment: A systematic review. J Psychopharmacol. 2025 Feb 13:2698811251319454. doi: 10.1177/02698811251319454.
Kondili LA et al. Inequities in primary liver cancer in Europe: The state of play. J Hepatol. 2024 Apr;80(4):645-660. doi: 10.1016/j.jhep.2023.12.031.
Zelber-Sagi S et al. One size does not fit all; practical, personal tailoring of the diet to NAFLD patients. Liver Int. 2022;42:1731-1750. doi: 10.1111/liv.15335.
Hadefi A et al. Dietary strategies in non-alcoholic fatty liver disease patients: From evidence to daily clinical practice, a systematic review. United European Gastroenterol J. 2023 Sep;11(7):663-689. doi: 10.1002/ueg2.12443. Epub 2023 Jul 25.
First steps nutrition trust. Ultra-Processed Foods marketed for infants and young children in the UK. 2023.
Vilar-Gomez E et al. PNPLA3 rs738409, environmental factors and liver-related mortality in the US population. J Hepatol. 2024 Oct 9;S0168-8278(24)02617-5. doi: 10.1016/j.jhep.2024.09.043.
Younossi ZM et al. Association of food insecurity with MASLD prevalence and liver-related mortality. J Hepatol. 2025 Feb;82(2):203-210. doi: 10.1016/j.jhep.2024.08.011.
Grinshpan LS et al. Ultra-processed food consumption and non-alcoholic fatty liver disease, metabolic syndrome and insulin resistance: A systematic review. JHEP Rep. 2023 Nov 17;6(1):100964. doi: 10.1016/j.jhepr.2023.100964.
Tirosh O et al. Differential effects of low or high-fat dairy and fat derived from dairy products on MASLD. JHEP Rep. 2024 Aug 22;6(11):101194. doi: 10.1016/j.jhepr.2024.101194.
Retat L et al. Preventing liver disease with policy measures to tackle alcohol consumption and obesity: The HEPAHEALTH II study. J Hepatol. 2024 Apr;80(4):543-552. doi: 10.1016/j.jhep.2023.11.021.
Manneville F et al. Associations between fruit and vegetable consumption and HCC occurrence in patients with liver cirrhosis. JHEP Rep. 2025 Feb 13. doi: 10.1016/j.jhepr.2025.101355.
Ren Z et al. Traditional lifestyle factors partly mediate the association of socioeconomic position with intrahepatic lipid content: The Maastricht study. JHEP Rep. 2023 Jul 18;5(11):100855. doi: 10.1016/j.jhepr.2023.100855.
Mucinski JM et al. Histological improvements following energy restriction and exercise: The role of insulin resistance in resolution of MASH. J Hepatol. 2024 Nov;81(5):781-793. doi: 10.1016/j.jhep.2024.06.017.




The World Liver Day activities carried out under the umbrella of Healthy Livers, Healthy Lives, are supported by Boehringer Ingelheim, Echosens, MSD, and Novo Nordisk. Our industry partners have had no input into the content of the World Liver Day activities.

